
We probably all know at least one person who swears by their magnetic charm bracelet for preventing travel sickness, reducing arthritic pain or even helping them through situations that induce an attack of social anxiety disorder. These bracelets and other devices (some are in the form of headbands, others pendants, blankets, knee braces, shoe inserts, there’s even one you wear in your pants to improve your sex life) use magnets of a similar strength to those that make shopping lists stick to your refrigerator or let your kids spell out rude words without you realising…
…in other words, they’re not very strong and so probably have absolutely no physiological effect whatsoever. So, this $5billion industry founded in ancient Greek mythology is almost on a par with homeopathy for having no real scientific basis. Or is it?
Serious research, being carried out in a serious university laboratory, with serious financial backing recently hit the headlines with proclamations that a short application of a magnetic field to an inflamed joint could somehow improve blood flow and reduce swelling. Thomas Skalak, chairman of biomedical engineering at the University of Virginia and his colleagues lead the field in the area of microcirculation research, the study of blood flow through the body’s tiniest blood vessels. This status presumably helped them secure $875,000 of US taxpayers’ money from the National Institutes of Health’s National Center for Complementary and Alternative Medicine.
Initially, they set out to examine a claim made by the companies that sell “therapeutic” magnets: that these devices somehow increase blood flow. Skalak’s team used magnets of 70 milliTesla (mT) field strength, which is about ten times stronger than a common refrigerator magnet, but still very weak, the magnetic field of an MRI machine, for instance, is up to about 3000 milliTesla (3 T in other words). The researchers measured blood vessel diameter before and after placing the magnets up against lab rats.
They found that the magnets seemingly had a significant effect on blood vessels. Those that had been dilated became narrower and those that were previously constricted widened. Apparently, this implies that the magnetic field could induce vessel relaxation in tissues with constrained blood supply, ultimately increasing blood flow; how the magnet knows which way to stimulate the effect is not known. In a more recent study, the team treated the hind paws of anaesthetized rats with inflammatory agents to simulate tissue injury. Therapeutic magnets were then applied to the swollen paws immediately. The researchers say they say significant reduction in swelling (oedema), although there was no effect if there was any delay between injury and application.
According to Skalak, “The FDA regulates specific claims of medical efficacy, but in general static magnetic fields are viewed as safe.” So, could magnets be used to improve blood flow following muscle injury, say, as many of the headlines surrounding this press release claimed?
Well, what I’d first like to know, is did the researchers use a double-blind control? Did they, for instance, apply non-magnetic objects of equal size, shape and weight and at the same temperature to a second set of inflamed rat hind paws to examine whether those had any effect on blood vessel dilation? Did they have a set of inflamed rats that were not treated at all? How did those groups respond? The research paper on which the press release is based was published online in November 2007 in the American Journal of Physiology and Heart Circulatory Physiology.
Given that one of the major tenets of sports injury treatment is ice and compression could it be that the very act of pressing an object against the inflamed joint simply acted as a compressive heatsink, reducing local temperature of the inflamed region and at the same time temporarily reducing blood flow during the compression?
It’s just a thought, but couldn’t any metallic object of a reasonable size, 10-20 mm would be adequate for a rat paw, act as a cold compress, asks my good friend Stephan Logan. Logan supplies scientific educational equipment, including neodymium rare earth magnets, and points out that these have a field strength of several thousand milliTesla (1.3 T is typical for the standard neo magnet N42) and so has a keen interest in scientific claims made about much weaker magnets, such as those used in the experiments, knowing that a nasty pinch when flesh is trapped between two neo magnets is one of the well-known physiological effects but has nothing to do with mystical field effects
The Virginia press release, and consequently much of the media, claim that since muscle bruising and joint sprains are the most common injuries worldwide, Skalak’s discovery has “significant implications”. He rightly points out that, “If an injury doesn’t swell, it will heal faster – and the person will experience less pain and better mobility.” The extrapolation of the magnetic research to the notion that “magnets could be used in much the same way ice packs and compression are now used for everyday sprains, bumps, and bruises, but with more beneficial results, is not necessarily supported.
Magnets could be used, but where is the evidence that they reduce swelling any more than a conventional cold compress? Indeed, does injecting a rat’s foot with an inflammatory chemical simulate adequately a sprain or strain? The release says, “The ready availability and low cost of this treatment could produce huge gains in worker productivity and quality of life.” That’s a big extrapolation from a small laboratory study to the whole of sports injury medicine. Anyway, if commercialised are these therapeutic magnet ever likely to be as cheap and readily available as a bag of frozen peas? I doubt it.


 We all know we’re all getting fatter, don’t we? Obesity has become the latest plague of the developed world. And, body mass index has become the vital statistic your GP is most interested.
We all know we’re all getting fatter, don’t we? Obesity has become the latest plague of the developed world. And, body mass index has become the vital statistic your GP is most interested.

 Does eating chocolate give you a headache? What about red wine? Cheese, perhaps? Yes, well read on to find out how a space-age detector developed to look for signs of life on Mars could soon become the kitchen gadget of choice for anyone who suffers a painful reaction to their food.
Does eating chocolate give you a headache? What about red wine? Cheese, perhaps? Yes, well read on to find out how a space-age detector developed to look for signs of life on Mars could soon become the kitchen gadget of choice for anyone who suffers a painful reaction to their food.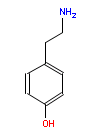 “Some foods have more biogenic amines than others,” explains Mathies, “but you cannot tell in advance because they aren’t listed on the food labels.” Even a single glass of wine has been known to trigger elevated blood pressure, heart rate and headaches in some people, he adds. He suggests that food manufactures and wine producers should be obliged to list biogenic amine content in their products by law. Although if they did, then this would preclude the need for the test kit, I assume, so the research team could concentrate on sending it to Mars instead.
“Some foods have more biogenic amines than others,” explains Mathies, “but you cannot tell in advance because they aren’t listed on the food labels.” Even a single glass of wine has been known to trigger elevated blood pressure, heart rate and headaches in some people, he adds. He suggests that food manufactures and wine producers should be obliged to list biogenic amine content in their products by law. Although if they did, then this would preclude the need for the test kit, I assume, so the research team could concentrate on sending it to Mars instead.